Do I really need to care about gingivitis?
Yes, you do need to care. We all do. But first, it's important to understand exactly what plaque is and how it is related to gingivitis.
What Is Plaque?
Plaque is a sticky, colorless film of bacteria that forms on your teeth every day. It develops when bacteria mix with food particles and saliva, especially along the gumline and between teeth. If plaque is not removed through regular brushing and flossing, it can build up, irritate the gums, and harden into tartar, which requires professional dental care to remove.
Plaque is where gingivitis begins.
What is gingivitis?
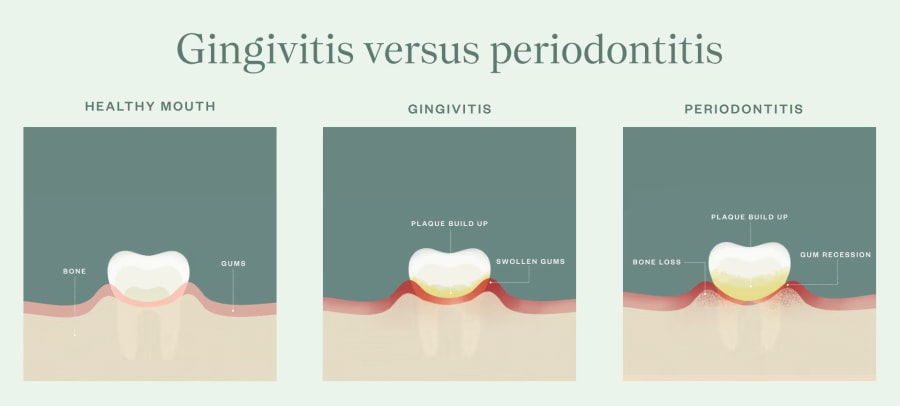
Gingivitis is the earliest and mildest form of gum disease. It happens when plaque builds up along and below the gumline, leading to gum inflammation. Common signs include redness, swelling, bleeding gums, and bad breath.
Because plaque forms every day, gingivitis is very common. In many cases, it can be managed with consistent brushing, flossing, and regular cleanings. But if it is not addressed, gingivitis can progress into periodontitis, a more serious and irreversible form of gum disease that may lead to bone loss, loose teeth, and tooth loss.
Catching it early keeps treatment simple and recovery smoother.
What causes gingivitis, and how does it develop?
So, how does gingivitis actually develop and progress? Gingivitis develops when plaque is not fully removed from along and below the gumline. As bacteria accumulate, the gums become irritated and inflammation occurs, often presenting early as redness, swelling, or bleeding gums during brushing.
If the plaque buildup isn't cleared away quickly with regular, thorough brushing and flossing, it will start to harden into tartar, which cannot be removed at home. Once tartar forms below the gumline, bacteria are better protected and inflammation becomes increasingly severe. Symptoms like persistent bleeding, tenderness, and bad breath from gum disease may become more noticeable.
The good news is that gingivitis is still treatable at this stage. With the right gingivitis treatment and consistent oral care, gum tissue can heal. But if inflammation is left to continue, your oral health can progressively deteriorate, with some very serious consequences.
What are some of the risk factors and lifestyle habits that impact gum health?
You brush your teeth regularly, but your dentist says you have gingivitis. What could the problem be?
All kinds of everyday factors influence how easily inflammation develops and how quickly gums recover. While brushing and flossing are essential, certain health conditions and habits can make gum inflammation more likely or harder to reverse.
Some common factors that increase the risk of gingivitis include:
- Smoking and gum disease: Smoking limits blood flow and slows natural gum tissue healing
- Diabetes and gingivitis risk: Diabetes can reduce immune response, making infection harder to control
- Hormonal changes and pregnancy gingivitis: Hormonal changes in pregnancy can make gums more sensitive to plaque
- Dry mouth caused by medications: Reduced saliva production can increase plaque production
- Long-term plaque exposure due to aging: Older people face a higher risk of gingivitis due to the natural aging process
Daily habits also play a role in overall gum health, including:
- Poor diet: Diets high in sugar and refined carbohydrates feed bacteria and contribute to plaque buildup
- Not drinking enough water: Poor hydration reduces saliva and allows bacteria to linger
- Inconsistent oral hygiene: Not brushing and flossing regularly allows plaque to accumulate and settle below the gumline
What are the early warning signs and symptoms to watch for?
The earliest signs of gingivitis are hard for most people to spot. But paying attention to small changes in your gums can help you catch gum disease early, when treatment is the most straightforward and most effective.
Early signs of gingivitis
The following symptoms may not seem like a big deal, but often signal the earliest stage of gum inflammation:
- Red or swollen gums
- Bleeding gums when brushing or flossing, even if it seems minor
- Tender or sensitive gum tissue
- Bad breath that does not improve with brushing
- A feeling that your gums are slightly puffy or irritated
At this stage, gingivitis treatment might simply be improved oral hygiene routines. Increased diligence when brushing and flossing, and remembering to clean your teeth at least twice a day, can often reverse inflammation completely. Daily brushing, flossing to prevent gingivitis, and professional cleanings all play a key role in gum tissue healing.
Signs of moderate gingivitis
When plaque buildup under the gums is left untreated, symptoms generally become more noticeable and persistent:
- Frequent or heavier bleeding when brushing
- Gums pulling away from the teeth, an early form of gum recession from gingivitis
- Increased tenderness or discomfort along the gumline
- Ongoing bad breath caused by bacteria trapped below the gums
- Early formation of periodontal pockets
These signs are a clear signal that gum inflammation is progressing and needs extra care from a dental professional. Taking action at this stage helps protect your gums, prevent further damage, and lower the risk of bone loss down the road.
What happens if I don’t treat gingivitis?
If left untreated, gingivitis can continue to advance until it becomes periodontal disease. This is a significantly more dangerous stage of gum disease that affects not only your gums but also the structures supporting your teeth. Periodontal disease is a serious threat to your oral and overall health. It can result in loose teeth, bone loss, or tooth loss and require surgery to treat.
Although gingivitis can often be reversed with non-surgical gum treatment and consistent care at home, periodontitis cannot. Once periodontitis has developed, there is no cure; the condition can only be managed. That’s why catching and treating gingivitis early, and keeping it in check over time, makes such a meaningful difference for your long-term gum health.
How does gum disease affect overall health?
Gum health is about more than your smile. When gingivitis is left untreated, bacteria and inflammation in the gums can affect the rest of the body, not just your mouth. As inflammation builds, oral bacteria can enter the bloodstream and place extra stress on your overall health.
Research shows a link between gum disease and heart health, with chronic inflammation playing a role in cardiovascular issues over time. There is also a close connection between diabetes and gingivitis risk, since each condition can make the other harder to manage without proper care.
Hormonal changes during pregnancy can make gums more sensitive to plaque, leading to pregnancy gingivitis. Untreated gum disease has been associated with pregnancy complications such as preterm birth and low birth weight, which is why preventive dental care is especially important during this stage of life.
Gum disease may also impact the immune system, making it harder for your body to fight off infections. The encouraging news is that with the help of your dentist and some diligent new oral hygiene habits, your gums can heal, and your overall health can benefit along with your smile.
How is gingivitis treated?
Gingivitis treatment focuses on gently removing the plaque and bacteria that irritate the gums, then helping keep them from coming back. The right approach depends on how early inflammation is caught and how much plaque buildup is present below the gumline.
When gingivitis is caught early, treatment often starts with a professional dental cleaning to remove plaque and tartar, paired with personalized guidance on brushing and flossing at home. For many people, this is all it takes to calm inflammation and get gums back to a healthy place.
If gingivitis has progressed, bacteria may be hiding deeper below the gums, where a routine cleaning cannot reach. In those cases, your dentist may recommend a deeper, non-surgical gum treatment to clean below the gumline and give your gums the opportunity to heal and reattach.
No matter the treatment plan, daily brushing and flossing play a big role in recovery. Consistent home care promotes healing, helps prevent gingivitis from returning, and keeps your gums feeling healthy between visits.
Professional treatment options
If bacteria have settled deeper below the gums, non-surgical gum treatment, such as scaling and root planing for gingivitis, may be recommended. This deep cleaning for gum disease removes tartar from periodontal pockets and smooths the tooth roots, allowing gums to heal and reattach more easily. The area is numbed for comfort during treatment, and afterwards, many patients notice reduced bleeding and healthier-looking gums as inflammation improves.
At Tend Dental, our dentists often recommend Perio Protect as part of ongoing care for patients with gingivitis. This treatment uses custom-fit trays to deliver medication below the gumline, targeting bacteria that brushing and rinsing cannot reach and helping maintain results between visits.

How long does non-surgical gum treatment take?
Because non-surgical gum treatment is more thorough than a typical cleaning, it requires more time to complete. Which means we may need you to schedule an extra visit, but the treatment is usually complete in one or two sessions. Similarly, because this treatment is more complex than a typical cleaning, it may not be fully covered by your insurance, and you may have a higher out-of-pocket cost.
We get that it’s not a great feeling to find out that you have to spend more time and money on a medical issue. (And, like any disease, gingivitis is a medical issue.) But, ignoring gingivitis will inevitably lead to more complex problems in the future that are far more time-consuming and expensive to deal with. We'll make every effort to help you avoid that.
READ MORE: My Dentist Said I Can't Get A Normal Cleaning. Why?
Should I see a periodontist?
Most cases of gingivitis can be managed with general dental care, but specialized treatment may be needed in certain situations. A referral to a periodontist is often recommended if you have deep periodontal pockets, signs of bone loss from gum disease, or gingivitis that does not improve with standard treatment.
Patients with systemic risk factors, such as diabetes, smoking, or immune-related conditions, may also benefit from periodontal care, as these factors can make gum disease harder to control. Seeing a specialist early helps protect gum stability and prevents more advanced complications.
How can I be sure I need this?
If you’re new to Tend and your prior dentist never diagnosed you with gingivitis, we know this can be a lot to process. Maybe you aren’t familiar with the warning signs and symptoms of gingivitis and aren’t sure whether the deep cleaning from non-surgical gum treatment is necessary. We want to assure you of two things.
First, Tend practices evidence-based dentistry that’s rooted in the latest clinical research. Advances in dental health science mean we now know more than we used to about gingivitis and how to treat it, and our team always adheres to the American Dental Association’s standards.
Second, our dentists don’t make a commission on procedures. They only offer the dental care you need. You can decide to proceed with any oral care treatment recommendations, confident that your interests and your dentist's are aligned.
How much does gum treatment cost?
The cost of gingivitis treatment can vary depending on how advanced the condition is and what type of care is needed. Early signs of gum disease are often addressed with routine cleanings and improved home care, while more advanced cases may require non-surgical gum treatment, such as scaling and root planing, which involves more time and specialized care.
Does insurance cover treatment for gum disease?
Dental insurance typically covers preventive services like regular cleanings and may offer partial coverage for deeper treatments when gum disease is diagnosed. Coverage varies by plan, so treatment recommendations are always based on clinical need first, with your dental team helping you understand insurance benefits and options along the way.
Gingivitis FAQs
-
Is gingivitis painful?
Gingivitis is not always painful, especially in the early stages. Many people only notice bleeding gums when brushing or persistent bad breath. The absence of pain does not mean gums are healthy, which is why regular dental visits are important for early diagnosis.
-
Can gingivitis cause bad breath?
Yes. Bad breath from gum disease is a common symptom of gingivitis. Bacteria trapped below the gumline release odors that brushing alone may not eliminate. Treating the underlying gum inflammation is the most effective way to improve breath long-term.
-
Can gingivitis turn into periodontitis?
Yes. If gingivitis is left untreated, it can progress into periodontitis. This happens when inflammation spreads deeper below the gumline, leading to periodontal pockets, gum recession, and bone loss from gum disease. Early gingivitis treatment helps prevent this progression.
-
Does gingivitis go away?
Yes, gingivitis can go away when it is caught early and treated properly. With professional gingivitis treatment, daily brushing and flossing, and regular dental cleanings, gum inflammation can fully resolve. If plaque buildup under the gums is not addressed, gingivitis will not go away on its own and may worsen over time.
-
Does mouthwash help gingivitis?
Mouthwash can help reduce bacteria and support gingivitis treatment, especially when used alongside brushing and flossing. However, mouthwash alone cannot remove plaque or tartar buildup under the gums. It works best as part of a complete oral care routine.
-
How can I prevent gingivitis?
Gingivitis prevention starts with daily brushing using fluoride toothpaste for gum disease prevention, flossing to prevent gingivitis, and using mouthwash for gingivitis as recommended by your dentist. Regular professional cleanings and avoiding smoking also play a key role in keeping gums healthy.
-
How long does gingivitis last?
How long gingivitis lasts depends on how quickly it is treated. Mild cases may improve within days to weeks once plaque is removed and proper home care begins. More advanced inflammation may take longer and require professional treatment, such as deep cleaning for gum disease.
-
How long does it take to reverse gingivitis?
In many cases, early signs of gum disease can begin to improve within one to two weeks of consistent brushing, flossing to prevent gingivitis, and professional cleaning. Full gum tissue healing may take several weeks, depending on the severity of inflammation and overall lifestyle and health factors like smoking or diabetes.
-
Is gingivitis bad?
While gingivitis is the mildest form of gum disease, it should not be ignored. If gingivitis is left untreated, it can progress to periodontitis, leading to periodontal pockets, gum recession, and bone loss from gum disease. Early treatment helps prevent long-term damage.
-
Is gingivitis curable?
Gingivitis is considered reversible rather than permanently curable. Once treated, gums can return to a healthy state, but gingivitis can come back if poor oral hygiene habits allow plaque and tartar to build up again. Ongoing care is key to long-term gum health.
-
What are the early signs of gingivitis?
Early signs of gingivitis often include red or swollen gums, bleeding gums when brushing or flossing, tenderness along the gumline, and bad breath from gum disease. These symptoms may be mild at first, which is why gingivitis is easy to overlook. Early detection makes treatment simpler and more effective.
-
What causes gingivitis?
Gingivitis is caused by plaque buildup under the gums. Plaque contains bacteria that irritate gum tissue when it is not removed through regular brushing and flossing. Poor oral hygiene habits, smoking, dry mouth, certain medications, pregnancy, and diabetes can all increase the risk of gum inflammation.
-
When should I see a dentist for gingivitis?
You should see a dentist if you notice bleeding gums when brushing, persistent bad breath, gum tenderness, or redness along the gumline. Early signs of gum disease are easier to treat and help prevent the need for more involved care later.
-
Will brushing teeth cure gingivitis?
Brushing alone is not enough to cure gingivitis, especially if tartar has already formed. Brushing twice daily with fluoride toothpaste for gum disease prevention is essential, but professional tartar removal and flossing are also necessary to fully treat gum inflammation. In more advanced cases, scaling and root planing for gingivitis may be required.
Schedule your gingivitis evaluation at Tend Dental
Healthy gums make a big difference, and you do not have to figure it out on your own. If you are noticing signs of gingivitis or just want peace of mind, our team at Tend is here to help. Book an appointment today and let us take care of your smile.